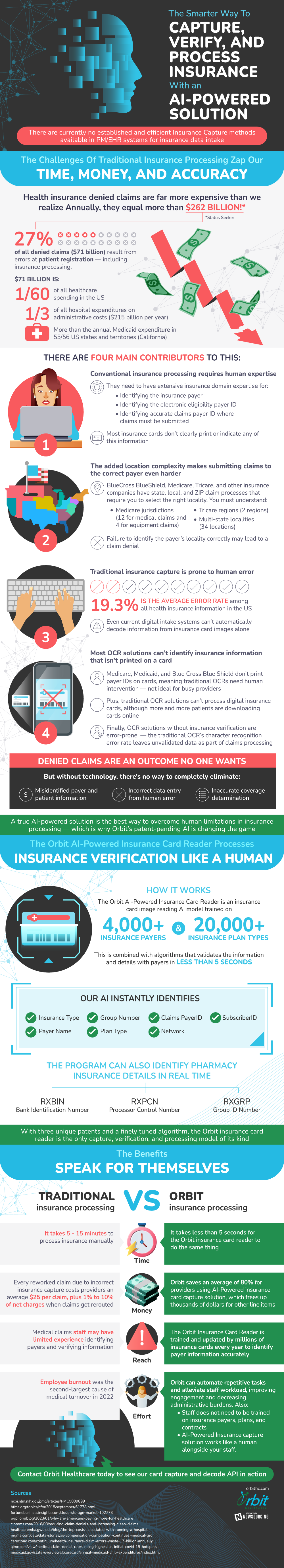
The Challenges Of Traditional Insurance Processing Zap Our Time, Money, And Accuracy
- Health insurance denied claims are far more expensive than we realize Annually, they equal more than $262 billion!* *Status Seeker
- 27% of all denied claims ($71 billion) result from errors at patient registration — including insurance processing
- $71 billion is:
- 1/60 of all healthcare spending in the US
- 1/3 of all hospital expenditures on administrative costs ($215 billion per year)
- More than the annual Medicaid expenditure in 55/56 US states and territories (California)
- There are four main contributors to this:
- Conventional insurance processing requires human experts
- They need to have expensive insurance domain expertise for:
- Identifying the insurance payer
- Identifying the electronic eligibility payer ID
- Identifying accurate claims payer ID where claims must be submitted
- Most insurance cards don’t clearly print or indicate any of this information
- The added location complexity makes submitting claims to the correct payer even harder
- BlueCross BlueShield, Medicare, Tricare, and other insurance companies have state, local, and ZIP claim processes that require you to select the right locality
- You must understand:
- Medicare jurisdictions (12 for medical claims and 4 for equipment claims)
- Tricare regions (2 regions)
- Multi-state localities (34 locations)
- Failure to identify the payer’s locality correctly may lead to a claim denial.
- Traditional insurance capture is prone to human error
- 3% is the average error rate among all health insurance information in the US
- Even current digital intake systems can’t automatically decode information from insurance card images alone
- Most OCR solutions can’t identify insurance information that isn’t printed on a card
- Medicare, Medicaid, and Blue Cross Blue Shield don’t print payer IDs on cards, meaning traditional OCRs need human intervention — not ideal for busy providers
- Plus, traditional OCR solutions can’t process digital insurance cards, although more and more patients are downloading cards online
- Finally, OCR solutions without insurance verification are error-prone
- The traditional OCR’s character recognition error rate leaves unvalidated data as part of claims processing
- Denied claims are an outcome no one wants
- But without technology, there’s no way to completely eliminate:
- Misidentified payer and patient information
- Incorrect data entry from human error
- Inaccurate coverage determination
A true AI-powered OCR solution is the best way to overcome human limitations in insurance processing — which is why Orbit’s patent-pending AI is changing the game
The Orbit AI-Powered Insurance Card Reader Decodes Payers, Records Plans, And Processes Insurance Verification Like A Human
- The Orbit AI-Powered Insurance Card Reader is an insurance card image reading AI model trained on 4,000+ insurance payers and 20,000+ insurance plan types
- This is combined with algorithms that validate the information and verify details with payers in less than 5 seconds
- Our AI instantly identifies:
- Insurance Type
- Payer Name
- Claims PayerID
- Plan Type
- SubscriberID
- Group Number
- Network
- The program can identify pharmacy insurance details in real time
- RXBIN: Bank Identification Number
- RXPCN: Processor Control Number
- RXGRP: Group ID Number
With three unique patents and a finely tuned algorithm, the Orbit insurance card reader is the only capture, verification, and processing model of its kind
And The Benefits Speak For Themselves
- Time
- It takes 5 - 15 minutes to process insurance manually
- It takes less than 5 seconds for the Orbit insurance card reader to do the same thing
- Money
- Every reworked claim due to incorrect insurance capture costs providers an average $25 per claim, plus 1% to 10% of net charges when claims get rerouted
- Orbit saves an average of 80% for providers using AI-Powered insurance card capture solution, which frees up thousands of dollars for other line items
- Reach
- Medical claims staff may have limited experience identifying payers and verifying information
- The Orbit Insurance Card Reader is trained and updated by millions of insurance cards every year.
- Effort
- Employee burnout was the second-largest cause of medical turnover in 2022
- With Orbit, you can automate repetitive tasks and alleviate staff workload, improving engagement and decreasing administrative burdens
- Staff does not need to be trained on insurance payers, plans, and contracts
- AI-Powered Insurance capture solution works like a human alongside your staff
Contact Orbit Healthcare today to see our card capture and decode API in action.
Sources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5009899/
https://www.carecloud.com/continuum/health-insurance-claim-errors-waste-17-billion-annually/
https://www.hfma.org/topics/hfm/2018/september/61778.html
https://www.ajmc.com/view/medical-claim-denial-rates-rising-highest-in-initial-covid-19-hotspots
https://www.mgma.com/data/data-stories/as-compensation-competition-continues,-medical-gro
https://www.ciproms.com/2016/08/reducing-claim-denials-and-increasing-clean-claims/
https://www.pgpf.org/blog/2023/01/why-are-americans-paying-more-for-healthcare
https://healthcaremba.gwu.edu/blog/the-top-costs-associated-with-running-a-hospital/
https://www.medicaid.gov/state-overviews/scorecard/annual-medicaid-chip-expenditures/index.html